Malaria and Maternal/Child Health in Africa

Every year, over 11 million pregnant women in Africa are infected with malaria, leading to devastating health consequences for both mother and child (WHO). Despite progress in prevention and treatment, malaria in pregnancy continues to be a major public health issue. It is not only a medical challenge but also a barrier to achieving the UN Sustainable Development Goals (SDGs) on maternal and child health.
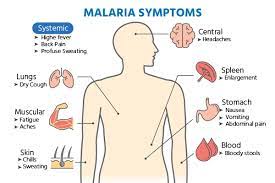
Why Malaria in Pregnancy is So Dangerous
Pregnant women are particularly vulnerable to malaria due to changes in their immune system. The risks include:
-
Maternal anemia – Severe malaria often leads to life-threatening anemia.
-
Stillbirths & Miscarriages – Malaria can cause fetal loss and pregnancy complications.
-
Low birth weight – One of the leading causes of infant mortality in Africa.
-
Increased maternal death – Malaria is a direct cause of maternal deaths in sub-Saharan Africa.
Children born to mothers infected with malaria face weakened immune systems, making them more prone to infections and stunted growth.
The Numbers Behind the Crisis
-
In 2022, 94% of malaria cases worldwide occurred in Africa.
-
Malaria in pregnancy was responsible for an estimated 819,000 low birth weight babies across sub-Saharan Africa (UNICEF).
-
In Nigeria alone, malaria is implicated in 11% of maternal deaths.
These numbers highlight why malaria in pregnancy is more than a health issue—it’s a developmental crisis.
Barriers to Prevention and Treatment
Several challenges worsen the situation:
-
Limited Access to Health Facilities – Many women in rural Africa lack access to antenatal care.
-
Low Awareness – Pregnant women may not know the importance of preventive malaria treatments.
-
Drug Resistance – Resistance to sulfadoxine-pyrimethamine (SP), used for preventive treatment, is emerging in some regions.
-
Cultural Beliefs – Misconceptions and reliance on traditional remedies often delay proper care.
Proven Solutions
Despite these challenges, effective strategies exist to reduce the burden of malaria in pregnancy:
-
Intermittent Preventive Treatment in Pregnancy (IPTp) – WHO recommends at least three doses of SP during pregnancy.
-
Insecticide-Treated Nets (ITNs) – Sleeping under treated nets reduces malaria risk by 50% or more.
-
Access to Antenatal Care – Early and regular checkups ensure malaria prevention and treatment.
-
Community Awareness Campaigns – Educating women and families about the risks and solutions.
Success Stories from Africa
-
Tanzania has scaled up IPTp, reaching over 70% coverage of pregnant women.
-
Ghana’s free distribution of ITNs has significantly reduced maternal malaria deaths.
-
Nigeria is piloting digital health platforms that remind women to take preventive malaria treatments during pregnancy.
These examples show that with political will and investment, progress is possible.
The Role of Technology and Innovation

Emerging technologies are reshaping maternal health and malaria prevention:
-
Mobile health (mHealth) apps send reminders to pregnant women about antenatal visits and malaria drugs.
-
AI-powered disease mapping predicts malaria hotspots, guiding targeted interventions.
-
Drone delivery systems are being tested in Rwanda to deliver malaria medicines to remote clinics.
Conclusion
Malaria in pregnancy is a silent killer that continues to claim the lives of African mothers and babies. The solutions are known—ITNs, preventive drugs, antenatal care, and education. What Africa needs is scaling up these interventions, supported by governments, international donors, and local communities.
At HubPharm Africa, we are committed to advancing maternal and child health by ensuring access to genuine medicines, education, and digital tools for women across the continent. Together, we can build a future where no mother or child dies from malaria.
Written by Fawzi Rufai, Medically Reviewed by Sesan Kareem